
A typical New Yorker walks more than 8,000 steps a day — but what happens when every step causes excruciating pain? This was what Charles*, a 40-year-old television editor in Manhattan, experienced when a herniated disc left him unable to sleep, work out, or even walk outside his apartment. Thanks to Dr. Ibrahim Hussain and his colleagues at Och Spine at NewYork-Presbyterian at the Weill Cornell Medicine Center for Comprehensive Spine Care, Charles is now back on his feet — but it was a long road.
“I woke up one morning feeling stiff,” Charles recalls. “At one point I sneezed, and then this pain started radiating from my lower back down to my foot. It hurt, but it was manageable; I was still able to walk around. It eventually went away, so I just thought I tweaked a muscle when I sneezed. But a couple months later, I did squats at the gym, and soon after, I started feeling that familiar pain from months ago. It worsened throughout the day, making it harder and harder to sit and work. I had to stretch and stand to make it through the day. I couldn’t even sleep; I woke up in the middle of the night in even more pain.”
Seeking relief for his back pain, Charles booked a massage therapist two blocks from his apartment, usually a two-minute walk. That day it took him 40 minutes. “I had to keep stopping and crouching down on the ground,” he says. “Worse, the session didn’t relieve my pain. I had to make that same walk home, and the pain kept getting worse. By that evening I was on my hands and knees on the floor — the only position where I experienced slightly less pain.”
The following morning Charles met with a physical therapist, who offered some relief. “She suspected a herniated disc might be the problem and showed me a position that I could lie down in that was comfortable enough to finally get some sleep,” says Charles. “Even with that, I still couldn’t walk, stand, or sit for more than a minute without feeling incredible pain. Around that time I started seeing Dr. Michelle Chi, a physical medicine and rehabilitation physician. The only way I could get there was to lie down flat in the back of an Uber.”
Dr. Chi, a partner at the Spine Center and also part of Och Spine at NewYork-Presbyterian/Weill Cornell Medical Center, ordered an MRI and an x-ray, which confirmed the presence of a very large herniated disc. A disc is said to herniate when the soft interior nucleus of one of the discs that serve as “shock absorbers” for the stacked bones of the spine (i.e., vertebrae) gets pushed out of its covering and presses onto a nerve. The pressure on the nerve can cause a multitude of issues, including weakness, numbness, or — as in Charles’ case — debilitating back and leg pain. Treatment generally starts with conservative measures, including physical therapy, steroids, and injections. In more severe cases, a surgical intervention is needed.
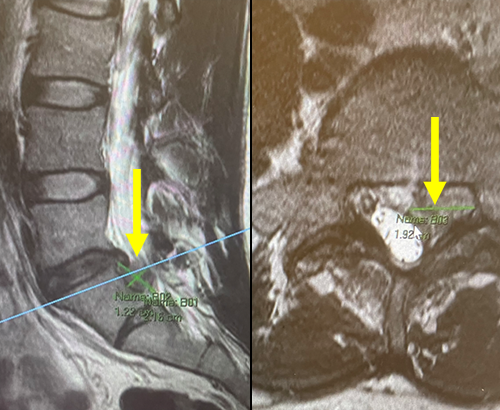
Scans showed the extent of the herniation Charles had experienced. The yellow arrow shows the large disc herniation that migrated and caused severe compression of a nerve root leading to classic symptoms of debilitating sciatica. At left, note the difference between the herniated disc and the healthy ones above it, which are all neatly contained in the intravertebral space.
“My colleague Dr. Chi, who I consider one of the most astute and conservative-minded specialists I work with, immediately referred Charles to me after seeing his imaging,” says Dr. Hussain. “When she sends me an urgent referral, I know it’s serious. Based on the images, which showed a severe herniation, we found that the only solution for Charles was a discectomy — removing the expelled part of the disc pushing on his nerve. Too much tissue had spilled out of the disk to allow us to consider physical therapy or epidural steroid injections, which could potentially cause more pressure and more pain. In consultation with Dr. Chi, we both agreed that that surgery was the best option for Charles. This is one of the unique benefits of working in a comprehensive spine center. Different specialists can coordinate care and recommendations on a case-by-case basis, many times in the same visit to save time and hassle for the patient.”
“After speaking with Dr. Hussain, I got second opinions just to be cautious,” says Charles. “But after I saw other doctors, Dr. Hussain stood out because he seemed to really enjoy his job. Where one neurosurgeon was cold, Dr. Hussain was compassionate, upbeat, helpful, communicative, and easy to talk to. Ultimately, I wanted someone who was more than just capable or with a good resume. I wanted someone who felt like they really cared about me as a human and wanted to see me do well. He answered all the questions I had, and based on his recommendation, I signed up for a discectomy feeling like I was in good hands.”
On the day of surgery, Charles arrived at NewYork-Presbyterian/Weill Cornell Medical Center feeling a little nervous, but he remembered some advice from a friend: "When you show up for surgery you don’t have to do anything,” Charles recalls. “Nothing’s on you and there’s nothing you can do to change the outcome. Just show up and let people do their job.”
Dr. Hussain’s approach was an ultra-minimally invasive endoscopic discectomy to remove the herniated portion of the disc. “Surgery for a herniated disc has come a long way,” says Dr. Hussain. “Before minimally invasive techniques were refined, surgeons would have to perform significantly more muscle cutting and bone drilling to gain access to the disc. Today, with endoscopic surgery, we make a tiny incision, less than half of an inch. We insert an endoscope equipped with a 4K high-definition camera lens that is a quarter of an inch in diameter, and guide it toward the affected disc herniation using X-ray or 3-dimensional computer navigation. In many cases, no muscle cutting or bone resection is required. Modified, extended surgical tools that fit down the same shaft are used to remove the herniation and confirm that pressure is taken off the nerve.”
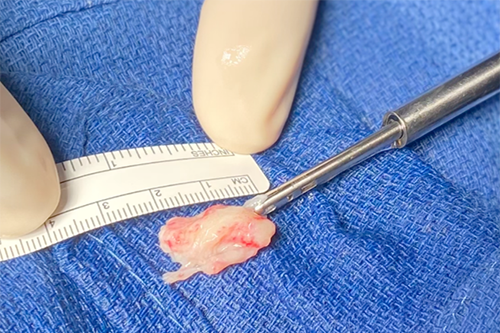
The herniated portion of the disc, which Dr. Hussain removed, measured more than 2cm in length. Although it appears small, it was in a space where there is only few a millimeters of room before severe nerve compression can occur.
Dr. Hussain had discussed the recovery process with Charles before the surgery — he would have some post-operative pain, to be managed by over-the-counter Tylenol, a muscle relaxer, and very limited opioids on an as-needed basis. He was also instructed to avoid what spine doctors call BLT (excessive bending, lifting, twisting) for six weeks while his spine recovered.
“When I woke up in recovery, I had pain all over my body,” recalls Charles. “When Dr. Hussain visited me in post-op, he told me that mine was one of the three most severe cases he’d ever done, in terms of the amount of herniated material he removed from the herniated disc.” Dr. Hussain even noted that the disc herniation could not even fit through the endoscope itself, so he had to perform an unorthodox maneuver and grasp the disc herniation tightly while removing the entire endoscopic system from Charles’ back.
“After an overnight stay, I was cleared to go home,” says Charles. “Once the six weeks had passed, I went into physical therapy, stretching and working core muscles to support my lower back. Gradually, I was able to start twisting and picking stuff up again. I just had to take it easy and slowly build my strength back up again.”
“A lot of friends and family told me not to get the surgery,” Charles says now. “But when you’re getting opinions about what you should or shouldn’t do, you have to keep in mind whose opinion it is. A neurosurgeon has an opinion that’s more qualified than your aunt or whoever. Ultimately, you have to gather as much quality information as possible and make the decision that’s right for you. The alternative to not having surgery is to wait a year and see if anything changes. But since I got the surgery, I was able to recover much faster. If you’re in debilitating pain, it’s worth entertaining the idea of getting surgery.”
Charles’ work in physical therapy has paid off: he’s back at the gym, he’s taken up jumping rope, and at least once a day he takes a nice long walk around Central Park — all things that the herniated disc once made unthinkable. There’s just one change, he says: No more squats!
*Patient prefers to use this pseudonym