
Karen Heimann, 62, a homemaker in New York City, spent her time doing “typical New York things” — visiting museums and art galleries, reading and watching movies, and taking care of Augie, her Irish Jack Russell Terrier. During the early days of the Covid-19 pandemic, Karen had settled into a routine, but her day-to-day life was disrupted when she woke up one Sunday with double vision. Life was far from normal for a while, but thanks to Dr. Theodore Schwartz and the team at Weill Cornell Medicine Neurological Surgery and NewYork-Presbyterian, Karen is back to living her life.
“I woke up from a Sunday afternoon nap seeing double,” she recalls. “Anything up close was fine, but anything further, such as the television, caused problems. My regular eye doctor wouldn’t be in on a weekend, so I called a friend for a favor. Her husband, an ophthalmologist, brought me to his office but couldn’t find anything wrong. He referred me to a retina specialist the next day. When I got to their practice, all the partners consulted on my case until the late afternoon. They couldn’t find anything either, which worried them — and me!”
Suspecting the problem might be in her brain, the doctors sent Karen to a neuro-ophthalmologist, who ordered an MRI scan. “Within a couple of hours, I had the results,” Karen sighed. “I took a look at the papers in the taxi on the way back to the doctor’s office. It felt like the longest ride ever.”
The MRI showed three tumors in Karen’s brain. One was “insignificant,” according to the neuro-ophthalmologist. The other two, however, were problematic, and one was the likely culprit behind her vision problems. The good news, so to speak, was that all three tumors appeared to be benign – but they should still be removed to resolve her symptoms.
“I was thankful it wasn’t cancer,” says Karen. “But my main concern was getting those two tumors out. I asked doctors and acquaintances for their recommendations. I had a lot of picks. There was one person in particular I trusted without question, a family friend since birth, whose brother-in-law is the head of a major medical center. He consulted with his head of neurosurgery, who said, ‘Without a doubt, not even a question: Ted Schwartz.’”

A pituitary adenoma is usually benign, but that doesn't mean it's harmless.
Karen visited NewYork-Presbyterian/Weill Cornell Medical Center to meet with Dr. Schwartz the following Friday. “He and his staff were really lovely,” she remembers. “And I felt like he really listened. He never blew me off, he was to the point, and he told me the facts. The most important thing to me was getting a great doctor who knew what to do.”
“Karen had three tumors, all of them benign,” says Dr. Schwartz. “A benign tumor is preferable to a malignant, cancerous one, but that doesn’t mean they’re harmless. One, a pituitary adenoma, was leaning on the optic nerve and causing her double vision. The other problematic one was a meningioma in an area on her left side that controlled her balance – she wasn’t having balance trouble yet, but eventually she would. Something had to be done about those two tumors, but the third could be monitored over time. Left unchecked, even benign tumors can cause further problems or, worse yet, create pressure in the skull that can cause further injuries to the brain or spine.”
The problematic tumors would need to be removed in two separate surgeries, Dr. Schwartz told Karen. “We targeted the pituitary tumor on her optic nerve first. Not only was that one causing symptoms, but it was in a location that could be reached with a minimally invasive surgery, allowing her to recover faster so we could schedule the second procedure, which would be more complicated.”
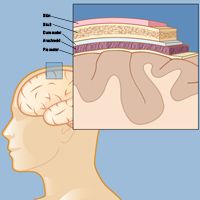
A meningioma is a tumor that develops in one of the protective layers around the brain and spinal cord, called the meninges. The meninges consist of the dura mater, the arachnoid membrane, and the pia mater, which lie directly below the skin and skull.
The pituitary tumor was removed endonasally – through a nostril, with the aid of an endoscope – one week after she was diagnosed.
“My team and I specialize in this type of surgery, which has revolutionized neurosurgery,” says Dr. Schwartz. “It involves threading a flexible tube through the patient’s nose and up to the area where the tumor is. The tube has a tiny camera attached, along with small surgical instruments. With this approach, we were able to remove Karen’s tumor with no cuts. The worst side effect most patients have to deal with is some sinus blockage.”
Ironically, Karen describes the blockage as the worst part. “When I woke up, my nose was completely clogged!” she laughs. “I love to talk, so it was unbearable for me.” Fortunately, the blockage resolved quickly, and she was ready for the second surgery.
“As soon as I was healed, I wanted to tackle the second tumor,” she says. “It was Covid, it was winter — why would I want this thing hanging over me? I just wanted to get it done and put it behind me.”
“We had to take a different approach for the second tumor, which was a meningioma,” says Dr. Schwartz. “Because of where it was situated, we couldn’t access it through the nasal passages. We performed a craniotomy, a procedure in which we remove a part of the skull to reach the brain and excise the tumor. Though this is a more invasive procedure, by definition, our goal is to cause as little strain on the patient’s body as possible, from incision to suture.”
After having two brain surgeries, Karen was pleasantly surprised at how smoothly everything went. “My experience was better than I could have imagined,” she says. “I spent two nights in the hospital for each operation. And honestly, I found the craniotomy easier to recover from! After the craniotomy, no one could even see that I’d had brain surgery unless I showed you the place Dr. Schwartz made his incision. After everything, I didn’t even feel like my head was cut open; the only thing I felt was a slight numbness.”
Though her pain was minimal, Karen’s body still had to recover. “I was almost back to myself in a week, but my recovery was gradual. I’d had two knee surgeries before, and you could track your recovery. Here, there was no metric to see how much I was improving, other than slowly feeling back to myself. There were days when I felt fine, but then I would exert myself and would be wiped out the following day. I had to allow my body to rest more than I thought. Slowly, I could do more and more around the house without getting tired. When I got to that point, I finally felt like myself again.In fact, after three months I was able to travel again, visiting both of my daughters that live outside of the New York area (one in San Francisco and one in Dublin).”

One memory, in particular, stands out to Karen. “What I found helpful for my recovery was being able to go home and shower after the craniotomy,” she recalls. “Getting out of the hospital clothes and into my own pajamas helped me feel better psychologically. These days, I’m fine — my neuro-ophthalmologist says I’m almost back to normal vision. He didn’t expect it to improve the way it did! And if I have to take care of the third tumor, there’s no question that I’d go back to Dr. Schwartz. I’d totally recommend him a hundred percent, both in terms of ability and who he is as a person. You want someone who’s beyond brilliant to operate on your brain, but you also want somebody who also listens to your concerns.”