
At age 79, Barbara Rothenberg is the matriarch of a large, tightknit family. She presides over eight successful children — seven lawyers and a pediatric nurse practitioner — as well as 50 grandkids and 17 great-grandchildren. As the managing partner for the Rothenberg Law Firm, Barbara works alongside her daughter Melissa Rothenberg-Kapustin, 42, who manages the firm’s Hackensack, New Jersey, office. Barbara and Melissa have a lot in common, including something not many mother-daughter pairs can claim: they were both treated by Dr. Theodore Schwartz at Weill Cornell Medicine Neurological Surgery for benign brain tumors, both meningiomas.
“Back in 2016, I started having headaches and was feeling very tired,” recalls Melissa. “I was losing a lot of weight. I’d just had my sixth child, and I chalked the headaches up to coaching basketball, soccer, and working full-time. I thought I just had too much on my plate, but I woke up one night and I couldn’t see out of my right eye. On top of that, my hearing in my right ear wasn’t 100 percent. Our firm handles traumatic brain injury cases, so with symptoms like these, I had some insight that I was dealing with some kind of neurological issue.”
What she never thought of was a brain tumor. A few years earlier, her mom had been diagnosed with a small meningioma when she went for a brain MRI for an unrelated issue. Barbara had no symptoms and had been advised to simply keep monitoring her meningioma. Melissa’s experience was so different that she never imagined it could be the same problem.
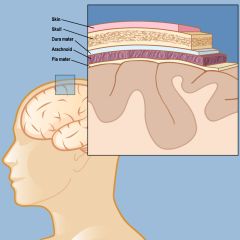
A meningioma forms in the meninges, the layers that include the dura mater, the arachnoid membrane, and the pia mater, which lie directly below the skin and skull.
“About ninety percent of meningiomas are benign and slow-growing, but they can present in different ways depending on the location and size of the tumor,” says Dr. Schwartz. “For Melissa, the sudden onset of symptoms was a result of tumor growth, when it started creating pressure in a part of her brain that affects vision. Other patients, like her mother, discover their meningioma incidentally. If the tumor isn’t causing any symptoms, it’s typical to schedule regular visits to monitor the meningioma’s growth, as Barbara did. It’s worth mentioning that, while researchers don’t fully understand what causes meningiomas, they are more common in women since they can respond to estrogen and progesterone.”
Seeking a diagnosis, Melissa turned to her brother, a fellow partner at the firm, for help in finding the right doctor. “I spoke to a Weill Cornell Medicine doctor who had worked with us on a legal case,” says Melissa. “She had helped advise on a client who had strep throat, was misdiagnosed, and subsequently suffered from neurological deficits. That doctor fit me into her schedule right away and had me undergo a brain MRI immediately after my visit with her. I thought the outcome would be like that strep patient since I had just recovered from a bad case of strep — that I would just need a strong course of antibiotics — but an MRI showed the meningioma. The neurologist was very kind and caring and she told me to immediately call Dr. Schwartz, and his team set up an appointment right away.”
“When there is a sudden onset of symptoms, it’s imperative to act quickly,” says Dr. Schwartz. “Once a tumor is pressing against nerves, blood vessels, or the brain itself, it could cause vision loss or, worse yet, create more severe neurological issues down the road. It’s critical to remove it quickly.”
A Surprising Schedule
Accustomed to thinking of a meningioma as something to monitor over time, Barbara was shocked by her daughter’s diagnosis and the recommendation for immediate surgery. “Things were moving fast, and I was very frightened for Melissa,” she recalls. “To go from finding the tumor to surgery, there was no time to think.”
Melissa, too, was taken aback. “I was floored that I could have a brain tumor,” she recalls. “At the time, I had a ten-month-old baby and five other kids at home. But Dr. Schwartz told me that things were going to be okay, that he would get me home to my baby. He was matter of fact about the potential for vision loss, and he explained to me in detail how much I needed the surgery. He was also very understanding. We had my daughter’s bat mitzvah coming up, but he told me not to worry, and we scheduled the surgery in ten days.”
The surgical approach for a meningioma depends largely on its size and location. “Melissa’s tumor, located behind her eyes in the base of the skull, allowed us to use a minimally invasive endonasal endoscopic approach,” says Dr. Schwartz. “That kind of procedure is an alternative to a craniotomy, where we open up the skull and excise the tumor. Instead, we thread a surgical endoscope right up through the nose to the tumor’s location and, using specialized tools, remove the meningioma without making any incisions.”
See animation of endonasal surgical approach
On the day of surgery, Melissa’s faith helped her on the nerve-racking walk from the pre-op room to the surgical suite. “We are Orthodox Jews, and every day when we wake up, we thank God for another day,” she says. “So once I got to that point before surgery, I just thought I was in God’s hands. And in Dr. Schwartz’s as His messenger. I just didn’t know if I would wake up and be able to see or hear or lose any of my other abilities.”
The surgery was a success — the tumor was removed and Melissa’s vision returned completely. An unfortunate complication from a cerebrospinal fluid leak left Melissa in the ICU for three days before she could go home, but that’s where having a big family paid off. “The whole family stepped up to make a rough recovery easier,” Melissa recalls. “One of my sisters took my kids home while I was in the hospital. And when I was at home resting, my eldest children took care of the youngest ones. My nine-year-old at the time, an aspiring doctor, was changing my bloody bandages and helping with my medication. My siblings visited me in the hospital and some even had a couple of their older children help out.”
The experience affected Melissa profoundly, and she became a mentor for the American Brain Tumor Association (ABTA). “I talk to people who are facing the same or similar surgery who don’t know where to go or don’t have someone to talk to. A lot of people go through the fear of the unknown when they get the diagnosis of a brain tumor. There is no question that brain surgery is terrifying, and it’s a valid fear. But now I’m on the other side of things and try to use my own experience to help others going through what I went through.”
Then It Was Mom’s Turn
That experience proved especially valuable when Barbara’s tumor suddenly reared its head. “My doctors in Philadelphia had been monitoring my meningioma year after year,” recalls Barbara. “Then in the spring of 2018 it got to a point where they said I needed surgery. I didn’t know enough about what the neurosurgeon in Philadelphia could do, but after what happened with Melissa, I knew what Dr. Schwartz could do!”
At that point Melissa had more than personal experience to offer. “By that time, I’d mentored several people at the ABTA, and I spoke to several people to whom I’d recommended Dr. Schwartz. Their stories about his care, in addition to my own experience, added to my confidence that my mother was in good hands.”
“Unlike Melissa’s tumor, Barbara’s meningioma was not in an area accessible via nasal passages,” says Dr. Schwartz. “This meant we couldn’t go the minimally invasive route, and our only option was to perform a craniotomy. Thankfully, the meningioma was close to the skull, so it was a less intensive surgery. It was as simple a craniotomy as could be — and one that, thankfully, she recovered from very quickly and gracefully.”
“My mother recovered in my house afterwards,” says Melissa. “After my own surgery, we were all ready to be caretakers. My siblings came to make sure she was okay, and their older kids helped out. My daughter who had helped with my bandages was helping her grandma with her stitches. One week after surgery, my book-loving mom was back shopping at Barnes and Noble.”
“Two successful surgeries were something to celebrate,” says Barbara. Melissa adds, “It’s what Jewish holidays are for! The first Hanukkah after our recovery, we celebrated our health and had a Seudat Hoda’ah, a meal of praise and thanks to God for helping us get through hard times.”
Melissa and Barbara both say they have more appreciation for their lives now. “Brain surgery is a terrifying thing,” says Melissa. “I say, ‘Thank God that it’s a benign meningioma — you can go on and live your life.’ I had another two children after brain surgery, and I’m back to working full time. My mother is fully capable and can spend time with her family. Some people hear ‘brain tumor’ and think it’s life-ending, but for a benign meningioma, be encouraged. And even if your experience is rough, be thankful that you can treat it and move on with your life.”
Barbara agrees. “If anybody called to ask me about Dr Schwartz, I’d say ‘you don’t want to have a brain tumor, but if you do, he’s the doctor to use!’”